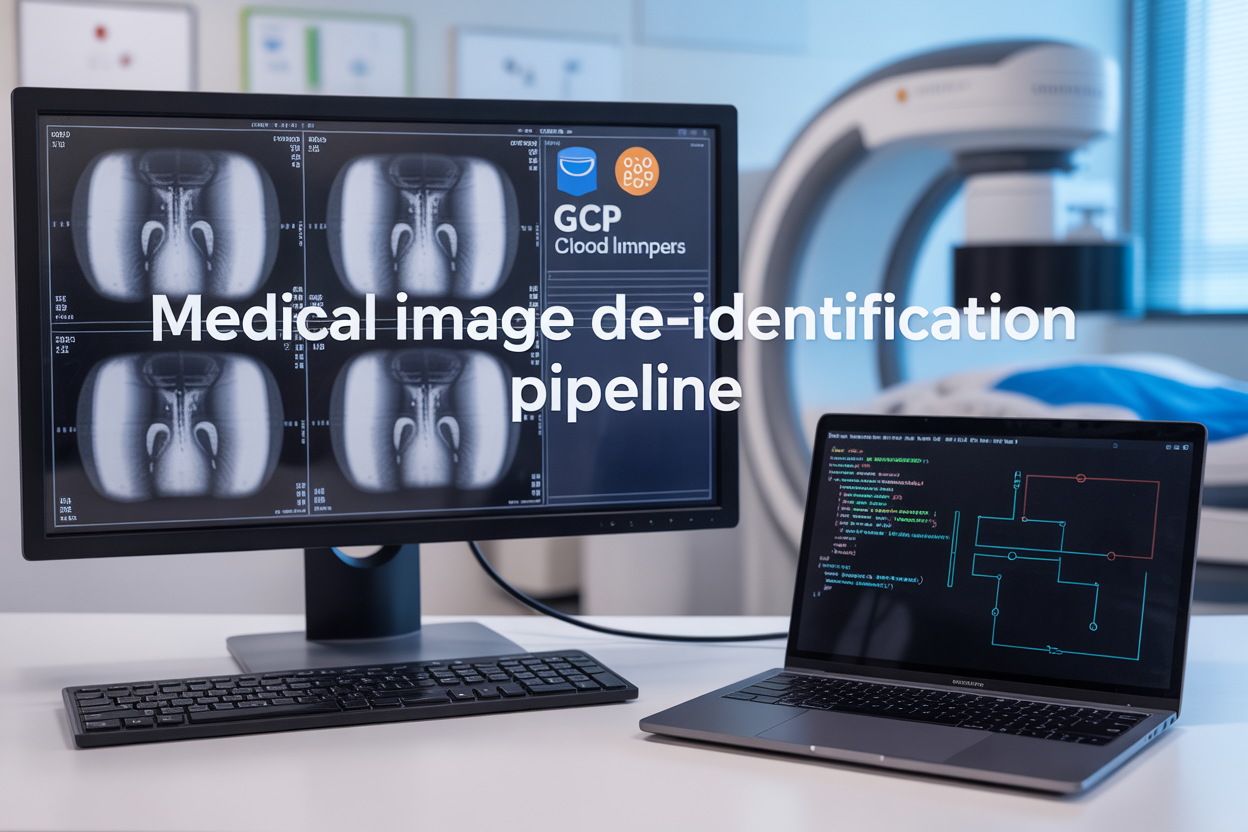
Protecting Patient Privacy in Medical Imaging with GCP’s Automated De-identification Pipeline
Medical imaging professionals, healthcare IT teams, and compliance officers face mounting pressure to protect patient privacy while maintaining diagnostic image quality. GCP medical image de-identification offers a robust solution through Docker healthcare image processing that automatically removes sensitive information from DICOM files and whole-slide images without compromising clinical value.
This comprehensive guide walks you through building and deploying a DICOM redaction pipeline that handles everything from metadata removal to visual redaction of burned-in text. You’ll learn how Google Cloud’s Healthcare API de-identification capabilities streamline compliance with HIPAA and other privacy regulations while processing thousands of images efficiently.
We’ll cover the technical architecture of a Docker-based pipeline that scales automatically, specific implementation strategies for both DICOM metadata removal and whole-slide image anonymization, and essential security measures that ensure your medical imaging data security meets industry standards. By the end, you’ll have a clear roadmap for implementing automated medical image redaction that protects patient privacy without slowing down your clinical workflows.
Understanding Medical Image De-identification Requirements
HIPAA Compliance Standards for Medical Imaging Data
HIPAA regulations create strict requirements for protecting patient health information in medical imaging systems. The Privacy Rule specifically addresses how organizations must handle protected health information (PHI) embedded in DICOM files and other medical images. Healthcare providers must implement administrative, physical, and technical safeguards when processing medical imaging data through GCP medical image de-identification pipelines.
The Security Rule establishes standards for protecting electronic PHI transmission and storage. Medical images often contain sensitive patient data beyond the visible diagnostic content, including metadata fields with patient names, medical record numbers, and treatment details. Organizations using Docker healthcare image processing solutions must ensure their de-identification workflows meet these federal standards.
HIPAA’s Minimum Necessary Rule requires limiting access to only the information needed for specific purposes. This principle directly impacts medical image privacy protection strategies, as automated redaction systems must identify and remove unnecessary PHI while preserving diagnostic value.
Privacy Risks in DICOM Metadata and Pixel Data
DICOM files present unique privacy challenges due to their complex structure containing both metadata and pixel data. The metadata includes over 200 standard fields that may contain PHI, such as patient demographics, study dates, referring physicians, and institutional information. Standard DICOM headers store information like PatientName, PatientID, StudyDate, and InstitutionName, all requiring careful handling during the de-identification process.
Pixel data poses additional risks through burned-in annotations, where text information becomes permanently embedded in the image pixels. These annotations might include patient identifiers, dates, or other sensitive information that traditional metadata scrubbing cannot address. Automated medical image redaction systems must employ optical character recognition and pattern detection to identify such embedded text.
Secondary capture objects and structured reports within DICOM files can contain free-text fields with unpredictable PHI. These elements require sophisticated natural language processing capabilities to detect and redact sensitive information effectively. Private DICOM tags used by specific vendors may also store PHI in non-standard locations, complicating the de-identification process.
Whole-Slide Image Annotation Vulnerabilities
Whole-slide images present distinct privacy challenges compared to traditional medical imaging formats. These high-resolution pathology images often contain specimen labels with patient identifiers, barcodes linking to medical records, and handwritten annotations that standard DICOM redaction pipeline solutions might miss.
The massive file sizes of whole-slide images require specialized processing approaches. A single slide can contain gigabytes of data, making real-time analysis computationally intensive. Whole-slide image anonymization processes must efficiently scan these large datasets while maintaining image quality for diagnostic purposes.
Annotation layers in whole-slide images may include pathologist comments, measurement data, and region-of-interest markings that could contain identifying information. These annotations exist as separate data structures within the image file, requiring specialized extraction and analysis tools. Healthcare API de-identification services must address these multi-layered data structures comprehensively.
Vendor-specific file formats like Aperio SVS, Leica SCN, or Hamamatsu NDPI each store metadata differently, creating additional complexity for standardized de-identification approaches. Cross-platform compatibility becomes essential when implementing automated redaction workflows.
Regulatory Framework Impact on Healthcare Organizations
Healthcare organizations face increasing regulatory pressure beyond HIPAA compliance. State privacy laws, international regulations like GDPR for global research collaborations, and FDA requirements for medical device software all influence medical imaging data security practices. These overlapping requirements create complex compliance landscapes that automated systems must navigate.
Audit requirements mandate detailed logging of all de-identification activities. Organizations must track which images were processed, what PHI was removed, and who accessed the de-identified data. GCP healthcare compliance pipeline implementations must provide comprehensive audit trails meeting these regulatory demands.
Risk assessment requirements force organizations to regularly evaluate their de-identification processes. This includes testing for re-identification risks, validating removal effectiveness, and updating procedures as new privacy threats emerge. The dynamic nature of privacy regulations requires flexible, updatable de-identification systems.
Breach notification requirements create additional pressure for robust de-identification. Organizations must demonstrate that proper de-identification reduces breach impact, potentially affecting notification timelines and penalties. Effective medical imaging data security becomes a critical component of overall compliance strategies.
GCP Healthcare API De-identification Capabilities

Built-in PHI Detection and Removal Features
Google Cloud Healthcare API offers comprehensive GCP medical image de-identification capabilities that automatically detect and remove Protected Health Information (PHI) from medical imaging data. The service recognizes common PHI elements including patient names, medical record numbers, dates, and physician identifiers embedded within DICOM metadata and image overlays.
The API employs sophisticated pattern matching algorithms to identify various PHI formats across different medical imaging modalities. For DICOM files, it automatically processes standard tags like Patient Name (0010,0010), Patient ID (0010,0020), and Study Date (0008,0020), while also scanning for burned-in text annotations that might contain sensitive information.
Key PHI detection capabilities include:
- Patient identifiers: Names, IDs, social security numbers
- Temporal data: Birth dates, study dates, acquisition timestamps
- Location information: Hospital names, department codes, room numbers
- Provider details: Physician names, technician IDs, referring doctor information
- Image overlays: Burned-in text containing patient demographics
The service provides flexible redaction options, allowing users to specify whether PHI should be completely removed, replaced with placeholder values, or anonymized using consistent pseudonyms. This DICOM metadata removal process maintains the structural integrity of medical images while ensuring compliance with healthcare privacy regulations.
Machine Learning-Powered Content Analysis
The Healthcare API leverages Google’s advanced machine learning models to perform intelligent content analysis that goes beyond simple pattern matching. These ML algorithms can identify PHI in unstructured text fields and image annotations that traditional rule-based systems might miss.
The ML-powered analysis excels at recognizing contextual PHI, such as patient information mentioned in radiology reports or clinical notes embedded within imaging studies. The system understands medical terminology and can differentiate between actual patient identifiers and similar-looking but non-sensitive data.
Advanced ML capabilities include:
- Natural Language Processing: Analyzes free-text fields in DICOM headers and reports
- Optical Character Recognition: Detects and redacts text burned into image pixels
- Contextual understanding: Distinguishes between PHI and medical terminology
- Multi-language support: Processes PHI in various languages commonly used in healthcare
- Confidence scoring: Provides reliability metrics for detected PHI elements
The automated medical image redaction process continuously improves through machine learning, adapting to new PHI patterns and imaging formats. This adaptive approach ensures consistent detection accuracy across diverse healthcare environments and imaging protocols.
Integration with Cloud Storage and Compute Services
The Healthcare API seamlessly integrates with Google Cloud’s storage and compute ecosystem, enabling scalable Docker healthcare image processing workflows. This integration supports both batch processing of archived medical images and real-time redaction of incoming studies.
Cloud Storage integration allows direct processing of DICOM files and whole-slide image anonymization without requiring local downloads. The API can process images stored in Cloud Storage buckets and output redacted versions to specified destinations, maintaining organized folder structures for different redaction policies.
Integration benefits include:
| Service | Capability | Use Case |
|---|---|---|
| Cloud Storage | Direct file processing | Batch redaction of archived studies |
| Compute Engine | Scalable processing power | High-volume image processing |
| Cloud Functions | Event-driven triggers | Automatic redaction on file upload |
| BigQuery | Analytics and reporting | PHI detection metrics and compliance reporting |
| Cloud Logging | Audit trails | Tracking redaction operations for compliance |
The GCP healthcare compliance pipeline architecture supports containerized deployments through Google Kubernetes Engine, enabling horizontal scaling based on processing demands. This cloud-native approach ensures consistent performance whether processing individual images or thousands of studies simultaneously.
Container orchestration capabilities allow teams to deploy custom redaction logic alongside the Healthcare API, creating hybrid workflows that combine Google’s ML-powered detection with organization-specific anonymization requirements. This flexibility makes the platform suitable for diverse healthcare environments with varying medical imaging data security needs.
Docker-Based Pipeline Architecture Benefits

Containerized Deployment for Scalable Processing
Docker containers transform how medical image de-identification pipelines operate by packaging entire environments into lightweight, portable units. When processing thousands of DICOM files or large whole-slide images, traditional deployments often struggle with resource allocation and dependency conflicts. Docker containers solve this by creating isolated environments where each processing task runs independently.
The GCP medical image de-identification pipeline benefits enormously from this approach. Containers can spin up automatically based on workload demands, processing multiple image batches simultaneously without interference. A single DICOM redaction pipeline container includes all necessary libraries, Healthcare API configurations, and processing scripts, eliminating the “it works on my machine” problem that plagues many medical imaging workflows.
Resource scaling becomes seamless with Kubernetes orchestration on Google Cloud Platform. When dealing with urgent patient data anonymization requests, additional container instances launch automatically to handle the workload. Each container processes its assigned batch of medical images while maintaining strict isolation for sensitive healthcare data.
Cross-Platform Compatibility and Portability
Docker healthcare image processing eliminates platform-specific deployment headaches that traditionally plague medical imaging systems. Whether running on Google Cloud Compute Engine, on-premises servers, or hybrid cloud environments, the same containerized de-identification pipeline operates consistently.
Medical institutions often maintain diverse IT infrastructures with different operating systems and hardware configurations. A Docker-based DICOM redaction pipeline runs identically across Windows servers in radiology departments, Linux machines in research facilities, and cloud instances handling overflow processing. This compatibility proves crucial when organizations need to migrate workloads or establish disaster recovery systems.
The portability extends beyond basic operating system differences. Container images package exact versions of image processing libraries, ensuring that DICOM metadata removal functions perform identically regardless of the underlying infrastructure. This consistency becomes vital for maintaining HIPAA compliance and audit trails across different deployment environments.
Automated Workflow Management
Container orchestration platforms enable sophisticated workflow automation that traditional medical image processing systems struggle to achieve. Docker containers communicate through well-defined APIs, allowing complex de-identification workflows to chain together seamlessly.
A typical automated workflow starts when new DICOM files arrive in a GCP storage bucket. Container-based triggers detect these files and launch appropriate processing containers. The pipeline automatically determines whether images require standard DICOM anonymization or specialized whole-slide image redaction strategies. Each processing step runs in its dedicated container, passing results to subsequent stages without manual intervention.
Error handling becomes more robust with containerized workflows. If a specific image processing container fails during metadata removal, the orchestration system automatically restarts that container without affecting other concurrent processing tasks. Failed jobs queue for retry with exponential backoff, ensuring that temporary issues don’t result in lost medical data or incomplete anonymization.
Monitoring and logging integrate naturally into the containerized architecture. Each container generates structured logs that feed into centralized monitoring systems, providing real-time visibility into de-identification progress and performance metrics.
Version Control and Reproducible Results
Docker images provide unprecedented control over medical image de-identification pipeline versions. Each container image represents a specific snapshot of processing code, dependencies, and configuration settings. This granular version control proves essential for maintaining audit trails and ensuring reproducible anonymization results.
Medical institutions can tag container images with specific version numbers, linking them directly to validation reports and compliance documentation. When regulatory audits require demonstrating exact processing steps used for patient data anonymization six months ago, teams can deploy the exact container version that handled those files.
Version rollbacks become straightforward when issues arise with updated de-identification algorithms. Instead of complex rollback procedures involving multiple system components, teams simply redeploy the previous container version. This capability reduces downtime and maintains continuous processing of urgent medical imaging requests.
Reproducible results extend beyond software versions to include exact processing environments. Container images capture not just application code but complete runtime environments, ensuring that DICOM redaction algorithms produce identical outputs when processing the same input files. This reproducibility supports research workflows where consistent anonymization across different processing runs is critical for data integrity.
DICOM Image Processing Implementation

Metadata Scrubbing and Tag Removal
DICOM files contain extensive metadata embedded within their headers, making DICOM metadata removal a critical first step in any de-identification pipeline. The GCP Healthcare API provides comprehensive tag removal capabilities that automatically identify and scrub personally identifiable information from over 100 standard DICOM tags.
The pipeline implementation focuses on both standard and private DICOM tags. Standard tags like Patient Name (0010,0010), Patient ID (0010,0020), and Study Date (0008,0020) require immediate removal or replacement with anonymized values. Private tags present additional challenges since manufacturers often embed proprietary information that could contain identifying details.
| Tag Category | Examples | De-identification Action |
|---|---|---|
| Patient Demographics | Patient Name, Birth Date, Sex | Remove or replace with coded values |
| Study Information | Study Date, Referring Physician | Shift dates, anonymize names |
| Equipment Data | Institution Name, Station Name | Remove or generalize |
| Private Tags | Manufacturer-specific fields | Complete removal recommended |
The Docker-based implementation leverages pydicom libraries alongside GCP’s Healthcare API to create a robust metadata scrubbing process. Custom validation rules ensure that no residual identifying information remains in the processed files while maintaining clinical relevance of the imagery.
Pixel Data Anonymization Techniques
Pixel-level anonymization goes beyond metadata removal to address identifying information burned directly into the image data. Medical image privacy protection requires sophisticated algorithms that can detect and redact text, faces, or other identifying marks while preserving diagnostic quality.
The pipeline employs multiple detection mechanisms including optical character recognition (OCR) for text identification and machine learning models for face detection. These techniques work together to create comprehensive pixel data protection without compromising the medical value of the images.
Key anonymization strategies include:
- Text overlay detection: Identifies patient information burned into images during acquisition
- Region-based redaction: Applies intelligent masking to specific anatomical regions
- Brightness and contrast normalization: Removes potential identifying patterns in image properties
- Histogram equalization: Ensures consistent image quality post-redaction
The Docker container includes pre-trained models optimized for medical imaging contexts, allowing for accurate detection while minimizing false positives that could unnecessarily obscure diagnostic information.
Burned-in Text Detection and Redaction
Burned-in text presents one of the most challenging aspects of DICOM redaction pipeline implementation. This text becomes part of the actual pixel data during image acquisition, making it invisible to standard metadata scrubbing techniques.
The detection process combines traditional computer vision approaches with modern deep learning models. OpenCV-based text detection algorithms work alongside TensorFlow models specifically trained on medical imaging datasets. This dual approach ensures high accuracy across different image modalities and text rendering styles.
The redaction process follows a multi-step workflow:
- Text localization: Identifies potential text regions using edge detection and morphological operations
- Character recognition: Applies OCR to verify actual text presence and content
- Sensitivity classification: Determines if detected text contains identifying information
- Intelligent redaction: Applies contextually appropriate masking techniques
The pipeline maintains a configurable sensitivity threshold, allowing healthcare organizations to balance privacy protection with diagnostic utility. Advanced inpainting algorithms fill redacted regions with statistically similar pixel patterns, ensuring seamless visual integration.
Series and Study Level De-identification
Automated medical image redaction extends beyond individual images to encompass entire study and series-level coordination. This comprehensive approach ensures consistent anonymization across related images while maintaining the clinical workflow relationships essential for diagnostic interpretation.
The pipeline implements hierarchical processing that begins at the study level, establishing consistent anonymization patterns across all constituent series. Cross-referencing algorithms ensure that related images receive identical de-identification treatments, preventing potential re-identification through cross-image correlation.
Study-level processing includes:
- Temporal consistency: Maintains relative timing relationships while anonymizing absolute timestamps
- Cross-series validation: Ensures consistent patient coding across different imaging modalities
- Referential integrity: Preserves study-to-series-to-image hierarchical relationships
- Batch processing optimization: Groups related images for efficient processing workflows
The Docker healthcare image processing container orchestrates these operations through configurable pipelines that adapt to different healthcare workflows. Integration with GCP’s Healthcare API enables scalable processing of large imaging datasets while maintaining audit trails for compliance verification.
Quality assurance mechanisms validate de-identification completeness across entire studies, flagging any inconsistencies or potential privacy leaks for manual review. This comprehensive approach ensures that the resulting anonymized datasets maintain clinical utility while providing robust privacy protection.
Whole-Slide Image Redaction Strategies
High-Resolution Pathology Image Challenges
Pathology whole-slide images present unique obstacles for medical image de-identification due to their massive file sizes, often reaching several gigabytes per image. These digital microscopy scans capture tissue samples at cellular resolution, creating files with dimensions that can exceed 100,000 pixels on each axis. The sheer data volume makes traditional image processing techniques inadequate, as loading entire images into memory would overwhelm most systems.
The complexity increases when considering that pathology images often contain multiple focal planes and magnification levels, creating pyramid structures with dozens of individual image layers. Each layer requires separate processing while maintaining consistency across the entire dataset. Patient information can be embedded at various levels within these hierarchical structures, from the base high-resolution layer to thumbnail previews.
Processing bottlenecks emerge when handling batch operations on multiple whole-slide images. Standard Docker containers may struggle with memory allocation and processing time, requiring specialized optimization strategies. The whole-slide image anonymization process must balance thoroughness with performance, ensuring complete privacy protection without creating prohibitively long processing times.
Color variations and staining artifacts in pathology images can interfere with text detection algorithms, making automated redaction more challenging than with standard medical imaging modalities. The microscopic nature of these images means that any remaining identifiable information could be virtually invisible to human reviewers but still machine-readable.
Annotation Layer Privacy Protection
Digital pathology workflows frequently include annotation layers containing physician markups, measurements, and diagnostic notes that may reference patient identifiers or sensitive clinical information. These overlay elements exist as separate data structures from the underlying tissue image, requiring targeted redaction strategies that preserve diagnostic value while ensuring medical image privacy protection.
Annotation metadata often contains timestamps, user credentials, and institutional information that can indirectly identify patients or reveal sensitive details about their treatment timeline. The GCP Healthcare API de-identification capabilities must extend beyond visible text to process XML-based annotation files, JSON structures, and proprietary markup formats used by different pathology software vendors.
Protected health information frequently appears in:
- Physician comments and diagnostic impressions
- Measurement labels and region descriptions
- Case study references and research protocol numbers
- Institution-specific coding systems and patient demographics
The Docker healthcare image processing pipeline must parse multiple annotation formats simultaneously while maintaining the spatial relationships between annotations and tissue regions. This process requires careful coordination between image processing and metadata sanitization to avoid corrupting the diagnostic integrity of the pathology review.
Version control becomes critical when managing annotation redaction, as pathology cases often undergo multiple review cycles with different specialists adding comments over time. Each annotation layer version must undergo the same rigorous de-identification process while preserving the chronological sequence of diagnostic findings.
Tile-Based Processing for Large Files
Breaking whole-slide images into manageable tiles represents the most effective approach for handling these massive datasets within Docker container constraints. This strategy divides images into smaller rectangular sections, typically 256×256 or 512×512 pixels, allowing parallel processing across multiple container instances while maintaining memory efficiency.
The automated medical image redaction pipeline implements intelligent tile boundary detection to prevent patient identifiers from being split across tile edges, which could compromise redaction completeness. Edge tiles receive special handling with overlap zones to ensure that text spanning tile boundaries gets properly detected and removed.
Processing orchestration becomes essential when coordinating hundreds or thousands of tiles from a single whole-slide image. The pipeline must track tile positions, processing status, and reconstruction order while maintaining data integrity throughout the workflow. Failed tile processing requires automatic retry mechanisms without affecting the overall batch operation.
| Tile Size | Memory Usage | Processing Speed | Detection Accuracy |
|---|---|---|---|
| 256×256 | Low | Fast | Good |
| 512×512 | Medium | Moderate | Better |
| 1024×1024 | High | Slow | Best |
Quality assurance measures include tile-level validation checks and seamless reconstruction verification. The final de-identified image must maintain the original resolution and color fidelity while ensuring complete removal of all identifiable information. Tile processing logs provide detailed audit trails for compliance documentation, tracking exactly which regions underwent redaction and the specific algorithms applied to each section.
The GCP healthcare compliance pipeline supports dynamic tile sizing based on image characteristics and available computational resources, optimizing processing efficiency for different pathology image types and institutional requirements.
Pipeline Deployment and Configuration
GCP Service Account Setup and Permissions
Setting up the right service account for your GCP medical image de-identification pipeline requires careful attention to security principles. Create a dedicated service account specifically for this pipeline rather than using default compute accounts. The service account needs several key permissions to function properly.
Start with Healthcare API permissions including healthcare.datasets.get, healthcare.dicomStores.dicomWebRead, and healthcare.dicomStores.dicomWebWrite. Add Cloud Storage permissions like storage.objects.get, storage.objects.create, and storage.buckets.get for handling input and output files. Include Cloud Run permissions such as run.services.get and run.services.update for container management.
Apply the principle of least privilege by granting only the minimum permissions needed. Consider using custom IAM roles instead of predefined broad roles. Enable audit logging for all service account activities to maintain compliance with healthcare regulations.
Required IAM Roles:
- Healthcare Dataset Editor
- Storage Object Admin (scoped to specific buckets)
- Cloud Run Developer
- Logging Writer
- Monitoring Metric Writer
Store service account keys securely using Google Secret Manager rather than embedding them in container images. Set up key rotation policies to refresh credentials regularly, typically every 90 days.
Docker Container Orchestration with Cloud Run
Cloud Run provides an excellent platform for orchestrating your DICOM redaction pipeline with automatic scaling and serverless benefits. Configure your container with appropriate resource limits based on image processing requirements. DICOM files typically require 2-4 GB of memory per concurrent request, while whole-slide images may need 8-16 GB.
Set up your Cloud Run service with these key configurations:
| Configuration | Recommended Value | Purpose |
|---|---|---|
| CPU | 2-4 vCPUs | DICOM processing |
| Memory | 4-8 GB | Image manipulation |
| Timeout | 15-30 minutes | Large file processing |
| Concurrency | 1-5 requests | Resource management |
| Max instances | 50-100 | Cost control |
Deploy using environment variables to pass configuration details like bucket names, Healthcare API endpoints, and processing parameters. This approach keeps sensitive information out of your container images and allows for easy configuration changes without rebuilding.
Enable Cloud Run revisions to maintain version control and enable quick rollbacks if issues arise. Use traffic splitting to test new versions safely before full deployment.
Configure VPC connectors if your Healthcare API datasets are in a private network. This ensures secure communication between your pipeline and protected health information systems.
Storage Bucket Configuration for Input and Output
Design your storage architecture with clear separation between input, processing, and output buckets. Create separate buckets for raw medical images, processed images, and audit logs. This separation improves security and makes data lifecycle management easier.
Configure input buckets with object change notifications that trigger your Cloud Run service automatically when new images arrive. Set up retention policies that automatically delete source files after successful processing to reduce storage costs and minimize data exposure.
Bucket Security Configuration:
- Enable uniform bucket-level access
- Apply customer-managed encryption keys (CMEK)
- Configure VPC Service Controls perimeter
- Set up bucket notifications for Cloud Pub/Sub
- Enable audit logging for all operations
Implement versioning on output buckets to track changes and maintain an audit trail. Configure lifecycle policies to automatically move older versions to cheaper storage classes or delete them after retention periods expire.
Set up regional buckets in the same region as your Cloud Run service to minimize latency and data transfer costs. Use multi-regional buckets only if you need global access to your de-identified images.
Monitoring and Logging Implementation
Comprehensive monitoring ensures your medical image de-identification pipeline operates reliably and meets compliance requirements. Set up Cloud Monitoring dashboards that track key metrics like processing time, success rates, and resource usage.
Create custom metrics for healthcare-specific monitoring:
- Processing latency per image type (DICOM vs. whole-slide)
- Redaction accuracy rates based on validation checks
- Failed processing counts with error categorization
- Data volume processed per hour/day
- Cost per image processed
Configure alerting policies that notify your team when processing fails, latency exceeds thresholds, or error rates spike. Set up escalation policies that page on-call engineers for critical failures affecting patient data processing.
Implement structured logging that captures all pipeline activities in a searchable format. Log entries should include processing timestamps, file identifiers, redaction operations performed, and any errors encountered.
Use Cloud Trace to monitor request flows across your pipeline components, helping identify bottlenecks in the medical image processing workflow.
Cost Optimization Strategies
Managing costs for your automated medical image redaction pipeline requires strategic resource planning and usage monitoring. Start by analyzing your processing patterns to understand peak usage times and adjust resource allocation accordingly.
Implement request batching to process multiple DICOM images in a single Cloud Run invocation, reducing cold start overhead. Configure your containers to handle multiple images per request when memory allows, optimizing CPU usage efficiency.
Cost Optimization Techniques:
- Use Spot VMs for non-urgent batch processing
- Implement intelligent scaling based on queue depth
- Configure minimum instances to reduce cold starts during peak hours
- Use committed use discounts for predictable workloads
- Archive processed images to cheaper storage classes
Set up budget alerts that warn when costs exceed expected thresholds. Create separate billing accounts or projects for different processing workflows to track costs more granularly.
Consider using Cloud Scheduler to run batch jobs during off-peak hours when Cloud Run pricing is most favorable. Implement queue-based processing that can buffer requests during high-demand periods and process them when resources are cheaper.
Monitor your Healthcare API usage carefully, as these costs can accumulate quickly with high-volume image processing. Consider caching frequently accessed metadata to reduce API calls.
Security and Quality Assurance Measures
End-to-End Encryption for Data in Transit
Medical image de-identification pipelines handle incredibly sensitive patient data, making robust encryption absolutely critical throughout the entire data journey. Your GCP medical image de-identification system should implement TLS 1.3 encryption for all API communications between Docker containers and Healthcare API endpoints. This ensures that DICOM files and whole-slide images remain protected while moving through your Docker healthcare image processing pipeline.
Google Cloud’s managed encryption keys provide seamless integration with your DICOM redaction pipeline. Configure your containers to use Cloud KMS for encrypting temporary storage volumes where medical images are processed. This approach prevents unauthorized access even if container instances are compromised during processing.
Network-level security becomes especially important when dealing with large whole-slide image files that may take considerable time to transfer. Implement VPC Service Controls to create security perimeters around your medical imaging data security infrastructure. This prevents data exfiltration attempts and ensures your automated medical image redaction workflow operates within controlled network boundaries.
Certificate pinning within your Docker containers adds another layer of protection against man-in-the-middle attacks. Your pipeline should validate SSL certificates at multiple checkpoints during the de-identification process, particularly when communicating with external healthcare systems or cloud storage repositories.
Validation Testing for De-identification Accuracy
Testing your medical image privacy protection system requires comprehensive validation strategies that go beyond basic functionality checks. Create test datasets containing synthetic medical images with known PHI patterns embedded in DICOM metadata, image pixels, and annotation layers. These controlled datasets allow you to measure de-identification accuracy rates and identify potential blind spots in your redaction algorithms.
Automated testing pipelines should validate multiple scenarios:
- Metadata Removal Verification: Check that all 18 HIPAA identifiers are completely removed from DICOM headers
- Pixel-Level PHI Detection: Test burned-in text detection across different image modalities and contrast levels
- Whole-Slide Image Annotations: Verify removal of pathologist annotations and embedded patient information
- File Integrity Validation: Ensure medical images remain diagnostically useful after processing
Cross-validation testing using holdout datasets helps identify overfitting in your Healthcare API de-identification configurations. Run your pipeline against images from different medical institutions, scanner manufacturers, and imaging protocols to ensure robust performance across diverse healthcare environments.
Performance regression testing catches degradations in de-identification quality when updating your Docker containers or modifying GCP healthcare compliance pipeline settings. Establish baseline accuracy metrics and trigger alerts when de-identification scores fall below acceptable thresholds.
Audit Trail Generation and Compliance Reporting
Your DICOM metadata removal system must generate comprehensive audit logs that satisfy healthcare regulatory requirements. Every image processed through your pipeline should create detailed records showing which de-identification methods were applied, what PHI was detected and removed, and verification that processing completed successfully.
Cloud Logging integration captures container-level events, API calls, and processing timestamps for complete traceability. Structure your logs to include:
| Log Component | Purpose | Retention Period |
|---|---|---|
| Processing Events | Track image flow through pipeline | 7 years |
| PHI Detection Logs | Document identified sensitive data | 7 years |
| Access Records | Monitor who processed which images | 7 years |
| Error Tracking | Capture failed de-identification attempts | 7 years |
Automated compliance reporting generates regular summaries for healthcare administrators and compliance officers. Your reporting dashboard should display de-identification success rates, processing volumes, detected PHI categories, and any anomalous patterns that might indicate system issues or security concerns.
Integration with Cloud Audit Logs provides immutable records of all administrative actions taken on your medical imaging infrastructure. This creates the paper trail necessary for HIPAA audits and regulatory compliance reviews. Configure log exports to secure, long-term storage systems that meet healthcare data retention requirements while maintaining cost efficiency for your automated medical image redaction operations.
Real-time monitoring alerts notify administrators immediately when de-identification processes fail or when unusual access patterns are detected. This proactive approach helps maintain the integrity of your medical image privacy protection system and ensures rapid response to potential security incidents.
Medical image de-identification has become a critical requirement for healthcare organizations working with patient data. We’ve explored how GCP’s Healthcare API provides powerful capabilities for removing sensitive information from DICOM and whole-slide images, while Docker containers offer the scalability and consistency needed for production environments. The combination creates a robust pipeline that can handle large volumes of medical images while maintaining strict security standards and ensuring regulatory compliance.
Setting up this redaction pipeline requires careful attention to both technical implementation and quality assurance measures. The Docker-based architecture makes deployment straightforward across different environments, while the built-in security features help protect patient privacy throughout the entire process. For healthcare teams looking to implement automated de-identification, start with a pilot project using a small dataset to test the pipeline configuration. This approach allows you to fine-tune the redaction strategies and validate output quality before scaling to full production workloads.